Oral Surgery

 Dental implants are changing the way people live. They are designed to provide a foundation for replacement teeth which look, feel and function like natural teeth. The person who has lost teeth regains the ability to eat virtually anything, knowing that the teeth appear natural and that facial contours will be preserved.
Dental implants are changing the way people live. They are designed to provide a foundation for replacement teeth which look, feel and function like natural teeth. The person who has lost teeth regains the ability to eat virtually anything, knowing that the teeth appear natural and that facial contours will be preserved.
What are Dental Implants?
 The implants themselves are tiny titanium posts, which are inserted into the jawbone where teeth are missing. These metal anchors act as tooth root substitutes. They are surgically placed into the jawbone. The bone bonds with the titanium, creating a strong foundation for artificial teeth. Small posts are then attached to the implant, which protrude through the gums. These posts provide stable anchors for artificial replacement teeth.
The implants themselves are tiny titanium posts, which are inserted into the jawbone where teeth are missing. These metal anchors act as tooth root substitutes. They are surgically placed into the jawbone. The bone bonds with the titanium, creating a strong foundation for artificial teeth. Small posts are then attached to the implant, which protrude through the gums. These posts provide stable anchors for artificial replacement teeth.
Benefits of Dental Implants:
- Improved appearance. Dental implants look and feel like your natural teeth.
- Improved speech. Dental implants allow you to speak without the worry that teeth might slip.
- Improved comfort. Since they become part of you, implants eliminate the discomfort of removable dentures.
- Easier eating. Dental implants function like natural teeth, allowing you to eat your favorite foods with confidence and without pain.
- Improved self-esteem. Dental implants can restore your smile and help you feel great.
- Improved oral health. More of your own teeth are left intact, improving long-term oral health. Individual implants also allow easier access between teeth, improving oral hygiene.
- Durability. With good care, many implants last a lifetime.
The Surgical Procedure
For most patients, the placement of dental implants involves two surgical procedures. First, implants are placed within your jawbone. For the first three to six months following surgery, the implants are beneath the surface of the gums gradually bonding with the jawbone. You should be able to wear temporary dentures and eat a soft diet during this time. At the same time, your dentist is forming new replacement teeth.
After the implant has bonded to the jawbone, the second phase begins. Our doctors will uncover the implants and attach small posts, which will act as anchors for the artificial teeth. These posts protrude through the gums. When the artificial teeth are placed, these posts will not be seen. The entire procedure usually takes six to eight months. Most patients experience minimal disruption in their daily life.
Are you a candidate for implants?
If you are considering implants, your mouth must be examined thoroughly and your medical and dental history reviewed. If you mouth is not ideal for implants, ways of improving outcome, such as bone grafting, may be recommended.
Surgical Advancements
Using the most recent advances in dental implant technology, our doctors are able to place single stage implants. These implants do not require a second procedure to uncover them, but do require a minimum of six weeks of healing time before artificial teeth are placed. There are even situations where the implants can be placed at the same time as a tooth extraction – further minimizing the number of surgical procedures. Advances in dental implant technology have made it possible, in select cases, to extract teeth and place implants with crowns at one visit. This procedure, called “immediate loading,” greatly simplifies the surgical process.
Major and Minor Bone Grafting
Over a period of time, the jawbone associated with missing teeth atrophies or is reabsorbed. This often leaves a condition in which there is poor quality and quantity of bone suitable for placement of dental implants. In these situations, most patients are not candidates for placement of dental implants.
Today, we have the ability to grow bone where needed. This not only gives us the opportunity to place implants of proper length and width, it also gives us a chance to restore functionality and esthetic appearance.
Major Bone Grafting
Bone grafting can repair implant sites with inadequate bone structure due to previous extractions, gum disease or injuries. The bone is either obtained from a tissue bank or your own bone is taken from the jaw, hip or tibia (below the knee.) Sinus bone grafts are also performed to replace bone in the posterior upper jaw. In addition, special membranes may be utilized that dissolve under the gum and protect the bone graft and encourage bone regeneration. This is called guided bone regeneration or guided tissue regeneration.
Major bone grafts are typically performed to repair defects of the jaws. These defects may arise as a result of traumatic injuries, tumor surgery, or congenital defects. Large defects are repaired using the patient’s own bone.
Sinus Lift Procedure
The maxillary sinuses are behind your cheeks and on top of the upper teeth. Sinuses are like empty rooms that have nothing in them. Some of the roots of the natural upper teeth extend up into the maxillary sinuses. When these upper teeth are removed, there is often just a thin wall of bone separating the maxillary sinus and the mouth. Dental implants need bone to hold them in place. When the sinus wall is very thin, it is impossible to place dental implants in this bone.
There is a solution and it’s called a sinus graft or sinus lift graft. The dental implant surgeon enters the sinus from where the upper teeth used to be. The sinus membrane is then lifted upward and donor bone is inserted into the floor of the sinus. Keep in mind that the floor of the sinus is the roof of the upper jaw. After several months of healing, the bone becomes part of the patient’s jaw and dental implants can be inserted and stabilized in this new sinus bone.
The sinus graft makes it possible for many patients to have dental implants when years ago there was no other option other than wearing loose dentures.
If enough bone between the upper jaw ridge and the bottom of the sinus is available to stabilize the implant, sinus augmentations and implant placement can sometimes be performed as a single procedure. If not enough bone is available, the Sinus Augmentation will have to be performed first, then the graft will have to mature for several months, depending upon the type of graft material used. Once the graft has matured, the implants can be placed.
Ridge Expansion
In severe cases, the ridge has been reabsorbed and a bone graft is placed to increase ridge height and/or width. This is a technique used to restore the lost bone dimension when the jaw ridge gets too thin to place conventional implants. In this procedure, the bony ridge of the jaw is literally expanded by mechanical means. Bone graft material can be placed and matured for a few months before placing the implant.
 Pre-prosthetic Surgery
Pre-prosthetic Surgery
The preparation of your mouth before the placement of a prosthesis is referred to as pre-prosthetic surgery.
Some patients require minor oral surgical procedures before receiving a partial or complete denture, in order to ensure the maximum level of comfort. A denture sits on the bone ridge, so it is very important that the bone is the proper shape and size. If a tooth needs to be extracted, the underlying bone might be left sharp and uneven. For the best fit of a denture, the bone might need to be smoothed out or reshaped. Occasionally, excess bone would need to be removed prior to denture insertion.
One or more of the following procedures might need to be performed in order to prepare your mouth for a denture:
- bone smoothing and reshaping
- removal of excess bone
- bone ridge reduction
- removal of excess gum tissue
- exposure of impacted teeth
- We will review your particular needs with you during your appointment
By the age of eighteen, the average adult has 32 teeth; 16 teeth on the top and 16 teeth on the bottom. Each tooth in the mouth has a specific name and function. The teeth in the front of the mouth (incisors, canine and bicuspid teeth) are ideal for grasping and biting food into smaller pieces. The back teeth or molar teeth are used to grind food up into a consistency suitable for swallowing.
The average mouth is made to hold only 28 teeth. It can be painful when 32 teeth try to fit in a mouth that holds only 28 teeth. These four other teeth are your Third Molars, also known as “wisdom teeth.”
Why Should I Remove My Wisdom Teeth?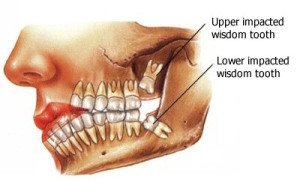
Wisdom teeth are the last teeth to erupt within the mouth. When they align properly and gum tissue is healthy, wisdom teeth do not have to be removed. Unfortunately, this does not generally happen. The extraction of wisdom teeth is necessary when they are prevented from properly erupting within the mouth. They may grow sideways, partially emerge from the gum and even remain trapped beneath the gum and bone. Impacted teeth can take many positions in the bone as they attempt to find a pathway that will allow them to erupt successfully.
These poorly positioned impacted teeth can cause many problems, including:
- Swelling, stiffness, pain and illness.
- The pressure from the erupting wisdom tooth may move other teeth and disrupt the orthodontic or natural alignment of teeth.
- Destruction of the jawbone and healthy teeth.
Oral Examination
With an oral examination and x-rays of the mouth, Dr. Adams can evaluate the position of the wisdom teeth and predict if there may be present or future problems. Studies have shown that early evaluation and treatment result in a superior outcome for the patient. Patients are generally first evaluated in the mid- teenage years by their dentist, orthodontist or by an oral and maxillofacial surgeon.
All outpatient surgery is performed under appropriate anesthesia to maximize patient comfort. Dr. Adams has the training, license and experience to provide various types of anesthesia for patients to select the best alternative.
Wisdom Tooth Removal
In most cases, the removal of wisdom teeth is performed under local anesthesia, laughing gas (nitrous oxide/oxygen analgesia) or general anesthesia. These options as well as the surgical risks (i.e. sensory nerve damager, sinus complications) will be discussed with you before the procedure is performed. Once the teeth are removed, the gum is sutured. To help control bleeding, you will bite down on the gauze placed in your mouth. You will rest under our supervision in the office until you are ready to be taken home. Upon discharge, your post-operative kit will include postoperative instructions, a prescription for pain medication, antibiotics and a follow-up appointment in one week for suture removal. If you have any questions, please do not hesitate to call us at 804-285-1378.
Our services are provided in an environment of optimum safety that utilizes modern monitoring equipment and staff that are experienced in anesthesia techniques.
Surgery For Impacted Canine Exposure
An impacted tooth simply means that is “stuck” and cannot erupt into function. Patients frequently develop problems with impacted third molar (wisdom) teeth. These teeth get “stuck” in the back of the jaw and can develop painful infections among a host of other problems. Since there is rarely a functional need for wisdom teeth, they are usually extracted if they develop problems. The maxillary cuspid (upper eye tooth) is the second most common tooth to become impacted. The cuspid tooth is a critical tooth in the dental arch and plays an important role in your “bite.” The cuspid teeth are very strong biting teeth which have the longest roots of any human teeth. They are designed to be the first teeth that touch when your jaws close together so they guide the rest of the teeth into the proper bite.
Early recognition of impacted canine is the key to successful treatment.
Recent studies have revealed that with early identification of impacted eye teeth (or any other impacted tooth other than wisdom teeth), treatment should be initiated at a younger age. Once the general dentist or hygienist identifies a potential eruption problem, the patient should be referred to the orthodontist for early evaluation. In some cases the patient will be sent to the oral surgeon before braces are even applied to the teeth.
The surgery to expose and bracket an impacted tooth is a very straight forward surgical procedure that is performed in the oral surgeon’s office. For most patients, it is performed with using laughing gas and local anesthesia. In selected cases it will be performed under IV sedation if the patient desires to be asleep, but this is generally not necessary for this procedure. The procedure is generally scheduled for 75 minutes if one tooth is being exposed and bracketed and 105 minutes if both sides require treatment. If the procedure only requires exposing the tooth with no bracketing, the time required will be shortened by about one half. These issues will be discussed in detail at your preoperative consultation with your doctor.
Click Here To View Images of Exposure and Bracketing of an Impacted Canine
TMJ (temporomandibular joint) disorders are a family of problems related to your complex jaw joint. If you have had symptoms like pain or a “clicking” sound, you’ll be glad to know that these problems are more easily diagnosed and treated than they were in the past.
These symptoms occur when the joints of the jaw and the chewing muscles (muscles of mastication) do not work together correctly.
TMJ stands for Temporomandibular Joint, which is the name for each joint (right and left) that connects your jaw to your skull. Since some types of TMJ problems can lead to more serious conditions, early detection and treatment are important.
No one treatment can resolve TMJ disorders completely and treatment takes time to become effective. Our doctors can help you have a healthier and more comfortable jaw.
 Trouble with Your Jaw?
Trouble with Your Jaw?
TMJ disorders develop for many reasons. You might clench or grind your teeth, tightening your jaw muscles and stressing your TM joint. You may have a damaged jaw joint due to injury or disease. Injuries and arthritis can damage the joint directly or stretch or tear the muscle ligaments. As a result, the disk, which is made of cartilage and functions as the “cushion” of the jaw joint, can slip out of position. Whatever the cause, the results may include a misaligned bite, pain, clicking or grating noise when you open your mouth or trouble opening your mouth wide.
Do you have TMJ?
- Are you aware of grinding or clenching your teeth?
- Do you wake up with sore, stiff muscles around your jaws?
- Do you have frequent headaches or neck aches?
- Does the pain get worse when you clench your teeth?
- Does stress make your clenching and pain worse?
- Does your jaw click, pop, grate, catch, or lock when you open your mouth?
- Is it difficult or painful to open your mouth, eat or yawn?
- Have you ever injured your neck, head or jaws?
- Have you had problems (such as arthritis) with other joints?
- Do you have teeth that no longer touch when you bite?
- Do your teeth meet differently from time to time?
- Is it hard to use your front teeth to bite or tear food?
- Are your teeth sensitive, loose, broken or worn?
The more times you answered “yes,” the more likely it is that you have a TMJ disorder. Understanding TMJ disorders will also help you understand how they are treated.
TMJ Treatment
There are various treatment options that our doctors can utilize to improve the harmony and function of your jaw. Once an evaluation confirms a diagnosis of TMJ disorder, our doctors will determine the proper course of treatment. It is important to note that treatment always works best with a team approach of self-care joined with professional care.
The initial goals are to relieve the muscle spasm and joint pain. This is usually accomplished with a pain reliever, anti-inflammatory or muscle relaxant. Steroids can be injected directly into the joints to reduce pain and inflammation. Self-care treatments can often be effective as well and include:
- Resting your jaw
- Keeping your teeth apart when you are not swallowing or eating
- Eating soft foods
- Applying ice and heat
- Exercising your jaw
- Practicing good posture
Stress management techniques such as biofeedback or physical therapy may also be recommended, as well as a temporary, clear plastic appliance known as a nightguard or splint. A night guard or splint fits over your top or bottom teeth and helps keep your teeth apart, thereby relaxing the muscles and reducing pain. There are different types of appliances used for different purposes. A nightguard helps you stop clenching or grinding your teeth and reduces muscle tension at night and helps to protect the cartilage and joint surfaces. An anterior positioning appliance moves your jaw forward, relives pressure on parts of your jaw and aids in disk repositioning. It may be worn 24 hours/day to help your jaw heal. An orthotic stabilization appliance is worn 24 hours or just at night to move your jaw into proper position. Appliances also help to protect from tooth wear.
What about bite correction or surgery?
If your TMJ disorder has caused problems with how your teeth fit together, you may need treatment such as bite adjustment (equilibration), orthodontics with or without jaw reconstruction, or restorative dental work. Surgical options such as arthroscopy and open joint repair restructuring are sometimes needed but are reserved for severe cases. Our doctors do not consider TMJ surgery unless the jaw can’t open, is dislocated and nonreducible, has severe degeneration, or the patient has undergone appliance treatment unsuccessfully.
What is Sleep Apnea?
People with obstructive sleep apnea (OSA) have disrupted sleep and low blood oxygen levels. When obstructive sleep apnea occurs, the tongue is sucked against the back of the throat. This blocks the upper airway and air flow stops. When the oxygen level in the brain becomes low enough, the sleeper partially awakens, the obstruction in the throat clears and the flow of air starts again, usually with a loud gasp.
Patients who suffer from sleep apnea often never reach REM sleep which is the most restful sleep, therefore they suffer from daytime sleepiness and lack of focus. In children, sleep apnea may result in hyperactivity, problems in school or bedwetting in older children. Untreated sleep apnea is one of the most undiagnosed conditions to date and can add to complications like heart attack, stroke, diabetes, heart failure, irregular heartbeat, obesity, Alzheimer’s disease, and premature death. Many motor vehicle accidents have occurred due to sleepy drivers.
There are Three Forms of Sleep Apnea
- Obstructive Sleep Apnea (OSA)
- Central Sleep Apnea (CSA)
- Mixed Sleep Apnea
As your dentist, we will ask you to fill out a sleep questionnaire. If the score indicates a probably of sleep apnea, our doctors will discuss testing options. A sleep test is the only way we’ll know for sure the level and type of apnea you have. Once results are reviewed by a Sleep Apnea physician, we can help explain the results and what level of care you need. We will often encourage you to share the results of the test with your primary care physician as they will also be part of your treatment plan team. Many treatments for OSA are available. CPAP (Continuous Positive Airway Pressure) is the most well-known but a dental appliance that you wear at night that will hold your jaw forward and help to keep your airway space open during sleep may also be an option. If an OSA dental appliance is an option for you, your dentist will discuss this with you. CSA must be treated by a sleep specialist and mixed sleep apnea may require other options as well.
Our goal in screening for sleep apnea is to provide you with the most comprehensive care possible in a dental office and reduce the numbers of untreated sleep apnea. Treatment is important for your health and your quality of life.
Common Symptoms of Sleep Apnea
- Loud, chronic snoring and long pauses in breath
- Choking or gasping while sleeping
- Feeling tired and sleepy throughout the day
- Waking up with a headache, dry mouth or sore throat
- Insomnia or constantly waking during the night
- Forgetfulness, irritability or depression
Silent Nite
In cases where patients suffer from severe snoring, but do not have sleep apnea, the silent night guard can help reduce snoring significantly. Silent Nite is flexible, thin and comfortable, and it exhibits documented clinical success in mitigating or even preventing the disruptive, unhealthy effects of snoring and sleep apnea. It moves the lower jaw into a forward position, increasing space in the airway tube and reducing air velocity and soft tissue vibration. The connectors are easily interchangeable by the patient.
Sleep Apnea Questionnaire
Based on the score of this questionnaire, our dentists will determine a patient’s probability of suffering from sleep related disturbances, and can suggest a home sleep study to confirm or rule out disturbances. Based on the results of the study our team and tailor a custom treatment plan to treat sleep apnea.



